Hyperlipidaemia
There are different types of lipoproteins that carry cholesterol and triglycerides in the blood. The main types include:
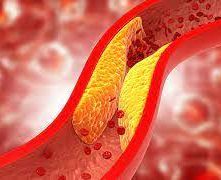
Low-density lipoprotein (LDL): Often referred to as "bad" cholesterol, high levels of LDL cholesterol are associated with an increased risk of cardiovascular disease. LDL cholesterol can deposit on the walls of arteries, forming plaques that narrow and stiffen the arteries, leading to atherosclerosis.
High-density lipoprotein (HDL): Known as "good" cholesterol, HDL helps remove LDL cholesterol from the bloodstream, reducing the risk of plaque formation. Higher levels of HDL are associated with a lower risk of cardiovascular disease.
Very-low-density lipoprotein (VLDL): VLDL carries triglycerides in the bloodstream. Elevated levels of VLDL are also associated with an increased risk of cardiovascular disease.
Hyperlipidaemia can result from various factors, including genetics, diet, lifestyle habits, certain medical conditions (such as diabetes, hypothyroidism, and kidney disease), and medications. Diets high in saturated fats, trans fats, and cholesterol can raise blood lipid levels. Lack of physical activity, smoking, excessive alcohol consumption, and obesity are also risk factors.
Hyperlipidaemia often does not cause noticeable symptoms on its own, so it's essential to have regular check-ups and lipid profile tests to monitor lipid levels. Treatment typically involves lifestyle modifications, such as adopting a heart-healthy diet, increasing physical activity, quitting smoking, and maintaining a healthy weight. In some cases, medication, such as statins, fibrates, bile acid sequestrants, or PCSK9 inhibitors, may be prescribed to help lower lipid levels and reduce cardiovascular risk.
Managing hyperlipidaemia is crucial for reducing the risk of cardiovascular complications. It requires a comprehensive approach that addresses both lifestyle factors and, if necessary, pharmacological interventions under the guidance of healthcare professionals.
How should we manage patients with hyperlipidaemia ?

Managing patients with hyperlipidaemia involves a comprehensive approach that includes lifestyle modifications and, if necessary, pharmacological interventions
Here's a general outline of how patients with hyperlipidaemia can be managed:
Hyperlipidaemia, also known as hyperlipidaemia or dyslipidaemia, refers to elevated levels of lipids (fats) in the blood. These lipids include cholesterol and triglycerides. Hyperlipidaemia is a significant risk factor for cardiovascular diseases, such as heart disease and stroke, which are leading causes of death worldwide.
1. Dietary modifications: Encourage patients to adopt a heart-healthy diet, such as the Mediterranean
diet or DASH (Dietary Approaches to Stop Hypertension) diet.
This includes:
- Limiting intake of saturated fats and trans fats found in red meat, full-fat dairy products, fried foods, and processed snacks.
- Increasing consumption of fruits, vegetables, whole grains, nuts, seeds, and lean proteins like fish and poultry.
- Encouraging foods rich in soluble fibre, such as oats, barley, beans, and lentils, which can help lower LDL cholesterol levels.
- Advising moderation in intake of cholesterol-rich foods, such as eggs and shellfish.
2. Regular physical activity: Encourage patients to engage in regular aerobic exercise, such as brisk
walking, jogging, cycling, or swimming. Aim for at least 150 minutes of moderate-intensity aerobic
activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening
activities on two or more days per week.
3. Weight management: For overweight or obese patients, weight loss can help improve lipid levels.
Aiming for gradual, sustainable weight loss through a combination of diet and exercise is
recommended.
4. Smoking cessation: Encourage patients who smoke to quit smoking, as smoking can worsen lipid
profiles and increase the risk of cardiovascular disease.
5. Alcohol moderation: If patients consume alcohol, advise moderation, as excessive alcohol intake can
raise triglyceride levels and contribute to other health problems.
6. Regular monitoring: Schedule regular follow-up appointments to monitor lipid levels and assess
progress. Adjust treatment plans as needed based on changes in lipid levels and overall
cardiovascular risk.
7. Pharmacological interventions: In some cases, lifestyle modifications may not be sufficient to
achieve target lipid levels, especially in patients with very high cardiovascular risk or genetic lipid
disorders. Pharmacological therapy may be recommended, including:
- Statins: These are the most commonly prescribed medications for lowering LDL cholesterol levels and reducing cardiovascular risk.
- Other lipid-lowering medications, such as ezetimibe, bile acid sequestrants, fibrates, and PCSK9 inhibitors, may be used alone or in combination with statins, depending on individual patient factors and treatment goals.
8. Management of comorbidities: Address and manage any underlying medical conditions, such as
diabetes, hypertension, or hypothyroidism, which can contribute to dyslipidaemia and increase
cardiovascular risk.
It's essential to individualise treatment plans based on each patient's specific lipid profile, overall cardiovascular risk, comorbidities, and preferences. Regular communication, education, and support from healthcare providers are crucial for successful management of hyperlipidaemia and reduction of cardiovascular risk.
Join us to understand how to manage your patients and achieve those QOF targets
Want to know more? Join us on one of our webinars BOOK HERE
For further information about our courses please contact us
Dovetail Team

